Zofran is generally considered safe for breastfeeding, according to most studies. It has minimal secretion into breast milk.
Understanding the balance between effective medication and breastfeeding safety is crucial for new mothers. Zofran, or ondansetron, often comes into the conversation for those needing nausea relief. This medication, widely used to prevent nausea and vomiting caused by chemotherapy, radiation therapy, and surgery, also finds its place in the regimen of breastfeeding mothers experiencing severe nausea.
Research indicates that Zofran’s presence in breast milk is minimal, making it a safer option than many alternatives. Mothers looking for relief from nausea while ensuring the well-being of their nursing infant might find Zofran to be a compatible solution. Always consult a healthcare provider before starting any new medication to ensure it aligns with your and your baby’s health needs.
Understanding Zofran
Many new moms wonder about the safety of medications while breastfeeding. Zofran, a medication commonly prescribed to treat nausea, often raises questions. Let’s dive into what Zofran is and its implications for breastfeeding mothers.
What Is Zofran?
Zofran, also known by its generic name ondansetron, is a prescription medication. It belongs to a class of drugs known as serotonin 5-HT3 receptor antagonists. Doctors often prescribe it to prevent nausea and vomiting caused by surgery, chemotherapy, or radiation therapy. It’s important to understand how Zofran interacts with the body, especially for breastfeeding moms.
- Designed to block chemicals in the body that trigger nausea and vomiting.
- Available in various forms, including tablets, dissolvable strips, and injectables.
- Generally well-tolerated with a proper prescription.
For breastfeeding mothers, the concern is whether Zofran passes into breast milk and its potential effects on the baby. The American Academy of Pediatrics considers Zofran usually compatible with breastfeeding, but it’s crucial to consult a healthcare provider.
Common Uses Of Zofran
Zofran serves a vital role in managing nausea and vomiting for various medical conditions. Its common uses include:
| Condition | Use of Zofran |
|---|---|
| Chemotherapy-induced nausea | To prevent nausea before and after treatment. |
| Postoperative nausea | To reduce the risk of vomiting after surgery. |
| Radiation therapy-induced nausea | To manage symptoms associated with radiation. |
| Severe morning sickness | As an off-label use for pregnant women with hyperemesis gravidarum. |
Understanding the medication’s uses helps determine its necessity and appropriateness for breastfeeding mothers. Always discuss with a healthcare provider before starting Zofran, particularly when breastfeeding.
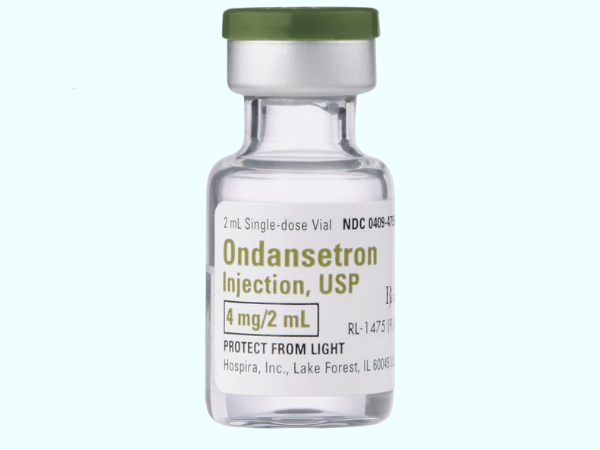
Therapy Zofran IV
Zofran IV ability to improve patient comfort significantly enhances the overall treatment experience, making it an essential tool in patient care.
How Does Zofran Work?
The way Zofran functions is quite specific. It targets certain areas in the brain and the gut. Here’s a simplified breakdown of its action:
- Blocks serotonin, a natural substance that causes vomiting.
- Acts on both central and peripheral nerves.
- Reduces the activity of the vagus nerve, which triggers nausea.
This targeted approach helps minimize nausea without many of the side effects associated with other anti-nausea medications. For breastfeeding moms, understanding Zofran’s action is crucial to ensure the safety of both mother and child.
Breastfeeding And Medications
When a new mother is breastfeeding, she often wonders about the safety of medications. Questions like “Is Zofran safe for breastfeeding?” are common. Zofran, or ondansetron, is a medication used to prevent nausea and vomiting. But is it safe for nursing mothers? Understanding how medications can affect breast milk and your baby is crucial. Let’s explore this important topic.
General Considerations For Breastfeeding Mothers
Nursing moms need to consider several factors before taking any medication, including Zofran. Medicines can pass into breast milk and affect the baby. Here are some general points to keep in mind:
- Consult your doctor before taking any medication, even over-the-counter ones.
- Read labels carefully to understand the active ingredients and potential side effects.
- Consider the age of your baby. Newborns process medications differently than older infants.
- Timing is key. Taking medicine right after breastfeeding might reduce its presence in the next feed.
- Monitor your baby for any signs of side effects or allergic reactions.
How Medications Can Transfer Into Breast Milk
It’s essential to know how and why medications transfer into breast milk. Here’s a brief overview:
Medications get into breast milk through the bloodstream. Once in the milk, they can pass to the baby during feeding. The amount that transfers can depend on several factors, including:
- The type of medication and its properties.
- The dosage taken by the mother.
- The frequency of the medication intake.
- The timing of the dose in relation to breastfeeding.
Most medications appear in breast milk at low levels. Yet, some can have adverse effects on a nursing infant. Always consult a healthcare provider for guidance.
Factors To Consider When Evaluating Medication Safety For Breastfeeding
Determining if a medication like Zofran is safe for breastfeeding involves several factors. Each factor plays a role in the overall safety for the nursing infant. Let’s look at some key considerations:
- Medication necessity: Is the medication essential for the mother’s health?
- Risk versus benefit: Does the benefit to the mother outweigh any potential risk to the baby?
- Medication alternatives: Are there safer options available that work just as well?
- Infant health status: Babies with certain conditions may be more sensitive to medications.
- Medication pharmacokinetics: How the body absorbs, uses, and eliminates the drug can affect its presence in breast milk.
Always discuss these points with a healthcare provider to ensure the best decision for both mother and baby.
Safety Of Zofran
Is Zofran Safe For Breastfeeding? New moms often ask this crucial question. Zofran, known generically as ondansetron, is a medication commonly used to prevent nausea and vomiting. Understanding the safety of Zofran during breastfeeding is vital. It ensures both mother and baby are at minimal risk while managing discomfort.
Research On Zofran And Breastfeeding
Thorough research is essential when considering any medication while breastfeeding. Ondansetron passes into breast milk in small amounts. Key studies highlight its effects:
- A study by the American Academy of Pediatrics deems it ‘usually compatible’ with breastfeeding.
- Data from the Drugs and Lactation Database (LactMed) suggests low levels in breastmilk.
- Minimal adverse effects have been reported in infants exposed to Zofran through milk.
Yet, research is ongoing, and long-term effects are not fully understood. Below is a summary of the current research insights:
| Study | Findings | Relevance |
|---|---|---|
| American Academy of Pediatrics | Usually compatible with breastfeeding | Suggests safety for infants |
| LactMed | Low levels in breastmilk | Indicates minimal infant exposure |
| Infant Exposure Reports | Few adverse effects | Supports the use with caution |
Potential Risks And Side Effects Of Zofran
While Zofran is effective for nausea, it is not without risks. Side effects can affect both the mother and the infant:
- Mother: Headache, constipation, and fatigue are common.
- Infant: Potential effects are less clear but could include irritability and changes in bowel movements.
More serious concerns include the rare risk of QT prolongation, a heart rhythm condition. This table outlines the potential side effects:
| Recipient | Common Side Effects | Serious Risks |
|---|---|---|
| Mother | Headache, constipation | QT prolongation |
| Infant | Irritability | Unknown long-term effects |
Safety Guidelines For Using Zofran While Breastfeeding
Mothers considering Zofran should follow these safety guidelines:
- Consult with a healthcare provider before starting Zofran.
- Use the lowest effective dose for the shortest time possible.
- Monitor the infant for any signs of side effects, like changes in behavior or bowel movements.
Always balance the benefits of nausea control against the potential risks. Maintain open communication with healthcare professionals to ensure the well-being of both mother and child.
Consulting A Healthcare Provider
Many breastfeeding mothers face the challenging decision of taking medications like Zofran. Concerns about safety for the nursing infant are paramount. Seeking guidance from a healthcare provider is crucial. They can offer personalized advice based on the latest research and your individual health needs.
Importance Of Professional Advice
When considering medication during breastfeeding, professional advice is key. Here’s why:
- Medication Transfer: Some drugs can transfer into breast milk and affect the baby.
- Infant Health: A healthcare provider can assess the risk to your infant.
- Individual Factors: Each mother and baby pair is unique. A professional can tailor advice to your situation.
- Latest Research: Healthcare providers have access to the most current information and can provide the best guidance.
Medications have different effects on different people. A table below shows factors that affect drug safety during breastfeeding:
| Factor | Details |
|---|---|
| Drug Properties | Size, solubility, and half-life of the medication. |
| Baby’s Age | Newborns are more vulnerable than older infants. |
| Mother’s Health | Conditions like liver function can affect drug metabolism. |
Discussing Zofran With Your Doctor
When you talk to your doctor about Zofran, consider these points:
- Your Symptoms: Share the severity and frequency of your nausea.
- Breastfeeding Goals: Discuss how long you plan to breastfeed.
- Medical History: Inform about past reactions to medications.
- Risks vs. Benefits: Understand the potential risks of Zofran to your baby compared to the benefits for you.
Ask questions to clarify any concerns. Your doctor might discuss:
- How Zofran works
- Possible side effects in infants
- Monitoring your baby for any adverse reactions
Keep a record of your discussion to refer back to if needed.
Alternatives To Zofran For Breastfeeding Mothers
If Zofran is not suitable, other options are available. Here are some alternatives:
- Dietary Changes: Small, frequent meals can help manage nausea.
- Hydration: Sipping fluids throughout the day prevents dehydration.
- Natural Remedies: Ginger or peppermint might ease symptoms.
Consider these non-pharmaceutical strategies:
- Acupuncture
- Aromatherapy
- Pressure point wristbands
Discuss all options with your healthcare provider to find the safest choice for you and your baby.
References
Discussing the safety of Zofran for breastfeeding requires careful consideration. Reliable references play a crucial role in such discussions. They provide the evidence and expert opinions needed to make informed decisions. This section delves into the research and guidelines from trusted medical sources.
Clinical Studies On Zofran And Lactation
Several clinical studies have examined Zofran’s effects on lactation. These studies offer insights into how the drug passes into breast milk and its potential impact on infants. Key findings include:
- Zofran’s transfer rate to breast milk.
- Effects on infant health and development.
- Recommendations for breastfeeding duration after Zofran administration.
Fda Guidelines On Zofran Use For Nursing Mothers
The U.S. Food and Drug Administration (FDA) provides guidelines on medication use for nursing mothers. These guidelines are based on risk assessment and clinical evidence. Important points include:
- Approved uses of Zofran for nursing women.
- Information on dosage and potential risks.
- Advice on monitoring infant reactions to Zofran exposure.
Expert Opinions From Healthcare Professionals
Healthcare professionals, including lactation consultants and pediatricians, provide valuable perspectives. Their opinions stem from clinical experience and research. Highlights encompass:
- Real-world observations on Zofran and breastfeeding safety.
- Risk-benefit analyses tailored to individual cases.
- Alternative treatments that may be safer for breastfeeding.